Autoimmune disorders - triggers & treatments we need to shout about!
The rise in Autoimmune disease is a health crisis.
There has been an exponential rise in autoimmune disorders (AID) over the last 50-70 years. Most AID were unheard of in 1970, and today there are between 100 and 140 recognised types of AID. The western world shows the most alarming increase, with estimates of 1 out of 7 people having an AID. American statistics show that around 50 million Americans currently suffer from autoimmunity – surpassing heart disease (22 million) and cancer (9 million), which we accept to be ‘the biggest killers’ (1.).
Some common AID are:
Coeliac disease
Rheumatoid arthritis
Asthma
Multiple sclerosis
Type 1 diabetes
Psoriasis
Hashimoto’s
Crohn’s
Ulcerative colitis
What leads to Autoimmune disease?
AID occurs when the immune system attacks the body’s own tissues. It usually progresses over time, but it can also seem to come on quickly when triggered by a significant and stressful health event. Conventional medicine usually treats AID by using pharmaceutical drugs to suppress the immune system and address disease symptoms. This is problematic, as the disease symptoms are just the signals the body sends, attempting to expose the deeper problem. Symptoms are important communication efforts, designed to prompt the sufferer to make necessary diet and/or lifestyle changes. When symptoms are masked by drugs but the root cause of the problem is not addressed, the human body will work around medications. Further symptoms will arise in other areas, signalling again to the sufferer to make necessary changes. If further medications are given for the new symptoms, the pattern repeats. This is how AID sufferers can find themselves accumulating multiple autoimmune diseases and in a situation of ‘poly-pharmacy’ (taking multiple drugs) when the necessary diet and lifestyle changes have not been made.
But isn’t autoimmunity caused by genes?
The way your genes express themselves is determined by the choices you make. If you have good health, but carry the autoimmune predisposition genes, then your choices have been supportive of good health. There are chemical, physical, and psychological contributions to gene expression. A gene’s role in disease manifestation is subject to the triggers that lead them to express, of which you have the power to affect. We see this in twins who carry the same AID predisposition genes, but having vastly different health pictures, and different backgrounds in terms of medications, antibiotic exposure, or other environmental factors.
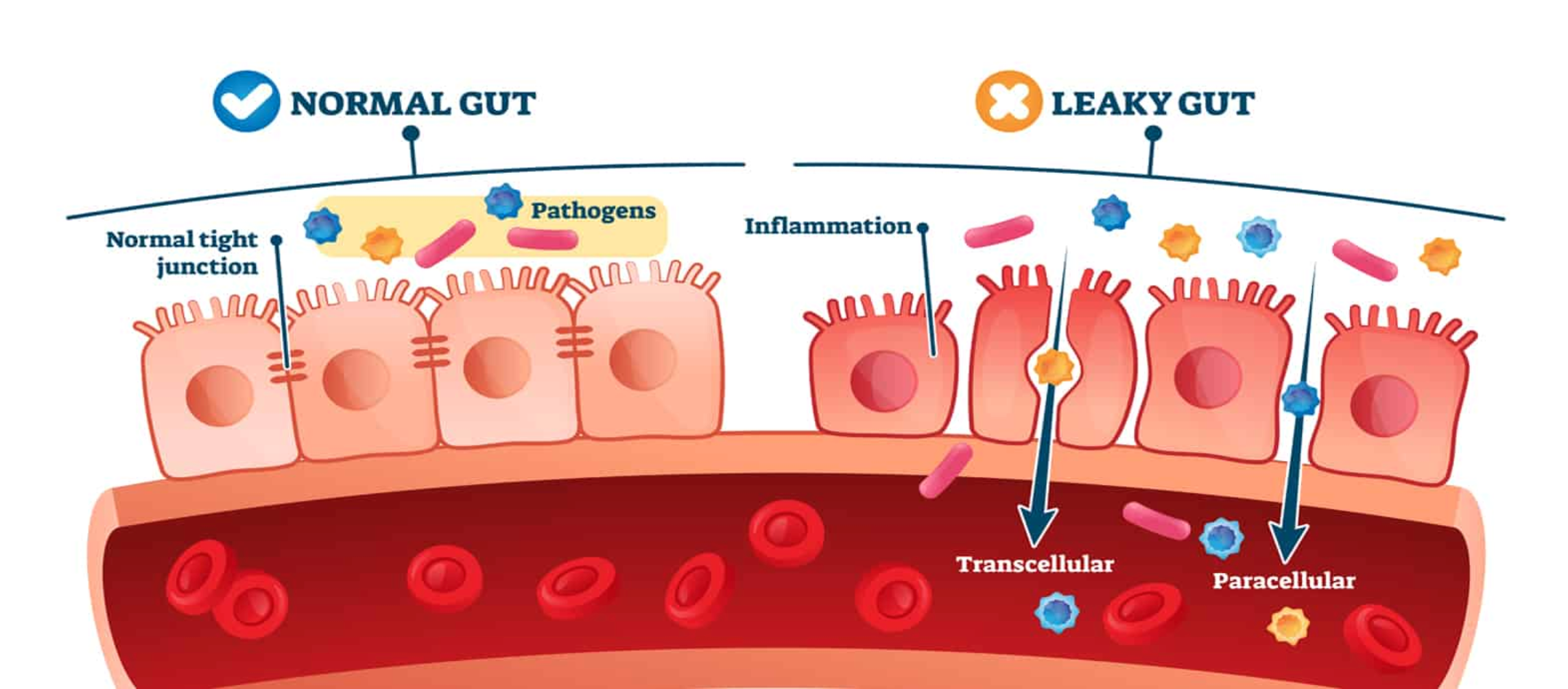
What is ‘leaky gut’?
Leaky gut, or intestinal hyper-permeability is the key precursor in AID progression. ‘Leaky gut’ might sound a bit amateur, but it plays a central role in AID. We know that 70 - 80% of your immune system resides in your gut. This is where immune cells are produced. So, it makes sense that damaging the gut implicates immune system malfunction.
Leaky gut means:
The immune system becomes overstimulated
Pathogens, toxins and unwanted proteins passing through the digestive tract can enter the bloodstream, and be distributed throughout the body.
Food sensitivities and allergies can develop.
Necessary absorption of nutrients, minerals, and vitamins is impaired, causing malnutrition.
The microbiome is affected, causing over-population of harmful microbes and insufficient populations of beneficial microbes.
Gastrointestinal tract is inflamed, potentiating disease.
Molecular mimicry is facilitated.
An overburdened immune system.
Inflammation is a necessary part of a healthy immune response. It eliminates pathogens and creates a hostile environment which prevents further invading pathogens. But chronic and abundant inflammation is harmful and leads to tissue damage aka leaky gut, and ‘molecular mimicry’. Molecular mimicry is facilitated by leaky gut. It implicates toxins or unwanted proteins entering the bloodstream, and then being mistaken for the cells of your own tissues. When the necessary changes to diet and lifestyle are not made, this perpetual state of immune system overwhelm, confusion and inflammation, results in disease manifestation.
Leaky gut & AID progression stages:
1. Gastrointestinal ecosystem triggers, eg:
a. Inflammatory foods
b. Pesticides
c. stress hormones
d. antibiotics
e. antacids and other medications
f. absorbed or inhaled toxins
g. insufficient exposure to microbes in nature (i.e. ‘too hygenic’)
h. metals
i. environmental chemicals
2. Overburdened immune system
3. Chronic consistent inflammation
4. Damaged gut wall tissue
5. Molecular mimicry
6. Autoimmune disease expression
Symptoms of this repair insufficiency can include fatigue, low energy, abdominal distention, stiffness, memory and cognition problems, easy bruising, constipation and/or diarrhoea, and general malaise. This can be easily dismissed, or medicated, when practitioners do not thoroughly investigate the individual’s health background, medication history, diet, lifestyle, toxic burdens, and other environmental factors. When root causes are not explored and then symptoms are masked with medications, the body deteriorates faster, and disease proliferates.
What does a gut need to be healthy, or to recover health?
A healthy gut requires the absence of inflammation, a diverse and healthy microbiome, robust intestinal walls for optimal nutrient absorption and barrier function, and the absence of tissue damage. When your gut is constantly harmed by dietary triggers, gluten, chemicals, antibiotics (and other medications), and other environmental factors, it becomes inflamed, damaged, and leaky.
The health of your gut microbiome.
A person’s gut microbiome (or gut microbiota) is highly individual, due to how they were born, feeding during infancy, where they grow up, the many contributing food, medication, and environmental factors throughout life. Two of the most influential factors on the health of your microbiome throughout life are how you were born (vaginal vs. caesarean), and type of feeding (breastfeeding vs. formula) (2.). Following this, big determinants of microbiome health are exposure to antibiotics and other medications, and exposure to processed inflammatory foods. Exposure to the mother’s vaginal biome through the birth canal during birth is an integral part of establishing the gut microbiome. Breast milk contains necessary bacteria and probiotics which help establish a diverse microbiome and robust immune system. The term ‘anti-biotics’ means ‘anti-life’, and as such, they kill all microbes, both the good and bad, making antibiotics one of the biggest microbiome threats. Processed inflammatory foods, chemicals inhaled or absorbed through your skin, other medications, metals, and other environmental toxins all contribute to microbiota demise, increasing risk and susceptibility for the autoimmune process to arise.
The role of food in autoimmune disease progression and reversal.
It is true what they say, ‘every single thing you eat or drink is either feeding disease or fighting it’. Addressing AIDs effectively requires figuring out the root causes and tailoring treatment protocols based on the persons health history and current health picture. One man’s food can be another man’s poison. Leaky gut is known to be multi-factorial, and individual cases are never the same. To determine individual causes of leaky gut it is best to work with a health practitioner that asks a lot of questions! However there are several common AID trigger foods, and several foods that have the power to heal when used correctly.
There is only one AID that conventional medicine has agreed on a prime cause – and that cause is FOOD, being coeliac disease and gluten. However, many natural health practitioners, doctors, and recovered AID sufferers will tell you that addressing gut health, diet, and lifestyle has a remarkable impact on reducing AID symptoms and facilitating recovery, whichever the specific type/s of AID they have been diagnosed with. Perhaps AIDs should not be classified as 100+ different conditions, but a ‘process’, inaugurated around chronically inflamed and permeable intestine walls. It’s one constitutive problem with many triggers that can differ between individuals, and develop or change over time.
A new approach to autoimmune disease.
If gut health is at the root of AID, then the right investigations, nutritional factors, and lifestyle changes, which we know can restore gut function, should be central to our AID approach. Testing for individual food sensitivities provides assistance with dietary considerations during the healing stages. These sensitivities can change and disappear as the integrity of the gut wall and diversity of the gut microbiome are improved, so re-testing periodically can be beneficial. Using a strategic dietary treatment plan can then help recover health in stages. Initially, a diet that is soft and gentle on the inflamed gut, and rich with the collagen and amino acids necessary to ‘heal and seal’ the intestinal wall (i.e., stop it leaking), is imperative to begin the restoration process. Then as gut wall integrity increases, various other foods can be reintroduced. The exclusion of any foods which sustain inflammation or are too difficult to digest is paramount to early gut-wall-restoration stages. Similarly, the exclusion of medications which directly or indirectly destroy the microbiome, e.g., antibiotics and antacids, is important. Then as AID symptoms improve, further nutrient dense and microbiome supporting foods can be introduced, at a careful and considered pace. As gut health improves, nutrient absorption from food increases, and the downward spiral of disease progression reverses into a healing succession.
Empowering yourself to get better
Your AID symptoms are an alarm bell, designed to incite changes to the daily diet and lifestyle factors which have led to health problems. Understanding this and being grateful for these alarm bells might be the first important step in regaining health. Appreciating that your body is clever enough to find a ‘back road’ around medications to present the signals somewhere else as additional symptoms is another element of your biological genius. Listening to these ques and paying attention to how things affect you is paramount. As body signals arise, respect your body by responding to them with considered change. Working with a nutritionist or naturopath who specialises in gut health is a great way to begin this journey.
To enquire about one on one online consults and support through your gut healing and/or autoimmune journey please email sarah@gutlabhealing.com. Face to face consults available at Torquay Chinese Medicine, hit the enquire button to book.